The federal government has revealed how it will spend $8.5 million on a number of test cases for the use of data from My Health Record as it continues efforts to justify the merits of the controversial scheme.
It comes just weeks before the three-month opt-out period for the electronic health record begins. From late October, every Australian will have a My Health Record (MHR) unless they have expressly chosen not to.
The government will be providing $600,000 each to 15 “testbed” projects using anonymised data from consenting MHR accounts in order to improve medical research and treatment.
The test cases include new ways of addressing and improving the efficiency of priority health areas using the digitised data.
The cases will only be able to use anonymised data from MHR users that consent to the use of their health information by secondary parties.
The selected test cases include efforts to improve patients’ engagement with pharmacists after being discharged from hospital, for better treatment of pancreatic cancer and for improved medical treatment of people transitioning from prison to the general community.
One of the chosen projects will be a trial run by Eastern Health and Monash University using MHR data to increase the engagement of patients and pharmacists after a discharge from hospital.
“These connections will allow healthcare providers to provide useful patient-specific information about medicines in the transition period from the hospital to the community.
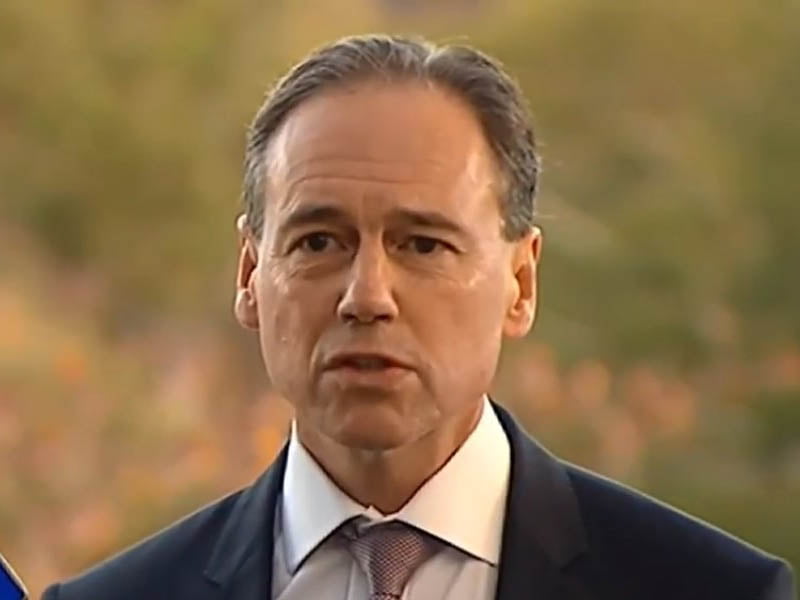
“We know when patients leave hospital on new medications they can find it confusing knowing how much to take and when,” Health Minister Greg Hunt said.
“Every year almost a quarter of a million Australians will be hospitalised from medication errors, which is more than the number hospitalised from car accidents.
“This program aims to reduce unplanned and early admissions to hospital due to medication errors while utilising evidence-based research.”
It’s another effort from the federal government to prove the worth of its highly controversial MHR scheme as the three month opt-out period fast approaches.
MHR has existed for five years as an opt-in service, with the government claiming that more than five million Australians already have a record.
The government is now moving to make the service an opt-out one, and provided $374.2 million over two years in the 2017 budget for the transition.
This switch has been labelled an “abuse of trust” by Australian Privacy Foundation health committee chair Dr Bernard Robertson-Dunn.
“This is a retrograde step. The government created the system as an opt-in and people made the decision to have one and consent was obtained. The government has then changed the rules to opt-out.
“Where is this going to stop? The government is abusing the trust of the people – they created a system to do one thing and then changed it because no-one was using it,” Dr Robertson-Dunn told InnovationAus.com earlier this year.
Dr Robertson-Dunn, along with a number of other digital and civil rights advocates, are encouraging Australians to opt-out of the system due to privacy and security concerns.
Many have argued that MHR could serve as a “honeypot” for potential hackers, with troves of valuable data stored in the one place.
There are also concerns that most Australians will not have even heard of MHR before the opt-out period is finished, meaning they will have no choice in the matter.
“The government is not going out of its way to tell people the full extent of this system. We are not impressed with the efforts the government is making to publicise this thing,” Dr Robertson-Dunn said.
The government has said that it is undertaking a national communication strategy to inform the public of the service before the opt-out period.
Australian Digital Health Agency CEO Tim Kelsey recently delivered a National Press Club address and defended the security of MHR.
“My Health Record operates to the highest cyber security standards and is independently audited on that basis by a number of organisations, including the Australian Signals Directorate.
“People are quite rightly concerned about the security of their clinical information but they are also concerned about how it might be used beyond their direct clinical care by governments and health researchers,” Mr Kelsey said.
“My Health Record has a range of protocols, which means that all instances of access by a clinician are attributable directly to them and recorded in real time.
“Unauthorised access is subject to a custodial prison sentence of up to two years. Trust is the essence of medicine – digital services can support confidentiality rather than undermine it.”
Do you know more? Contact James Riley via Email.

