Australia’s most powerful doctors’ group is urging the Commonwealth to clarify the contradictions between its assertions that no medical information will be passed on to authorities with a warrant and the actual legislation underpinning it.
Australian Medical Association president Tony Bartone told the National Press Club last week that he would meet with Health Minister Greg Hunt, calling on government to do “whatever it takes” to remove the ambiguity currently surrounding the MHR service, including potentially amending the legislation.
While Mr Hunt and the agency behind MHR, the Australian Digital Health Agency, have maintained that no sensitive data stored on the electronic record would be handed over to authorities without a warrant, this requirement is not reflected in the legislation.
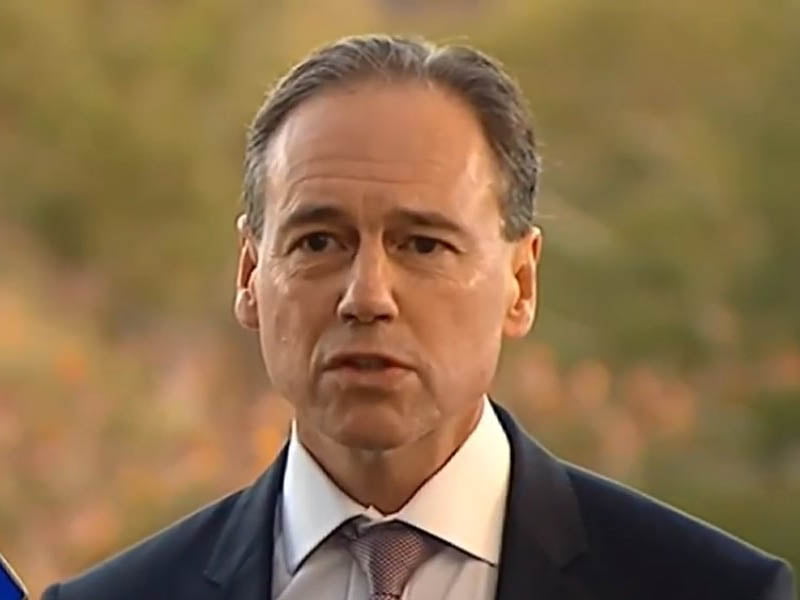
Mr Hunt and the ADHA’s claims have also been extraordinary rebutted by the Parliamentary Library.
Section 70 of the My Health Record Act says that the agency only has to “reasonably believe” that the release of data is “reasonably necessary” to assist with the prevention, detection, prosecution or punishment of a criminal offence, for the enforcement of laws or the “protection of the public revenue”.
The government has maintained that the ADHA’s own policy overrides this, and no data would be handed over without a court-issued order.
Dr Bartone said he shared many of the concerns about the potential for authorities to access data stored on MHR, and the contradictions between the legislation and the ADHA’s policies.
He said he had received a written assurance from Mr Hunt that no information would be accessed on the system without a “court ordering or judicial oversight”. But Dr Bartone said more must be done.
“I will ensure that any ambiguity in the differences between what the legislation says and the practicality of the interpretation are crystal clear and there can be no ambiguity for our members and the public going forward,” Dr Bartone said during the Press Club address.
“Anything which impairs or creates ambiguity between what the legislation says and the assurances that I’ve received in writing must not be allowed to occur. I’ve made it clear that I will be seeking a meeting with the minister to ensure that any ambiguity is put to rest, and whatever measures need to be done to make sure that this is once and for all put to bed.”
Dr Bartone confirmed that the actual legislation may need to be amended to properly address his concerns.
“I’ll be having a conversation with the minister and if it means we have to go there, that’s where we’ll go,” he said.
“I am sure the government is committed to a successful rollout of this and anything that gets in the way of the trust in the system by doctors will be seen as a deal-breaker, and that will be dealt with accordingly and appropriately.”
Dr Bartone would also raise the “protection of the public revenue” clause with the minister.
“The entire section of the legislation will be a subject of the conversation. It’ll be important to understand exactly where and where not, and must be clearly in the public interest and be at the same level that exists currently now, and that’s only with a court order or judicial oversight,” Dr Bartone said.
It comes after the Parliamentary Library last week sensationally contradicted these claims in a blog post by the director of the foreign affairs, defence and security section Nigel Brew.
In the post, the Parliamentary Library said that section 70 “represents a significant reduction in the legal threshold for the release of private medical information to law enforcement”.
“Although it has been reported that the ADHA’s ‘operating policy is to release information only where the request is subject to judicial oversight’, the My Health Records Act 2012 does not mandate this and it does not appear that the AHA’s operating policy is supported by any rule or regulation,” Mr Brew said in the post.
“As legislation would normally take precedence over an agency’s ‘operating policy’, this means that unless the ADHA has deemed a request unreasonable, it cannot routinely require a law enforcement body to get a warrant, and its operating policy can be ignored or changed at any time.
“The health minister’s assertions that no one’s data can be used to ‘criminalise’ them and that ‘the Digital Health Agency has again reaffirmed today that material…can only be accessed with a court order’ seems at odds with the legislation which only requires a reasonable belief that disclosure of a person’s data is reasonably necessary to prevent, detect, investigate or prosecute a criminal offence.”
The Parliamentary Library did acknowledge that the provision was in the original legislation passed by the previous Labor government and “received little attention when the bill was debated”.
Speaking to the media on Wednesday, Mr Hunt hit back at the Parliamentary Library’s claims.
“There’s an error in that analysis and that is that the clear, unchanging, absolute unconditional policy and practice of the Digital Health Agency is to implement that to the standard of a court order. That will remain the position, I think, forever,” Mr Hunt said.
“There’s been a six-year period up until now, and we now have approximately six million people on record, no materials, not one document has been released to the policy.
“The policy implementation and interpretation of that is that there will not be any document ever released without a court order, which is the standard.”
During his speech, Dr Bartone said MHR has had a “very difficult inception” over more than a decade.
“It’s been a very difficult birth and transition over the course of the journey. There has been a lot of effort and goodwill expended in setting up this system,” he said.
“It’s not the best possible system as it currently stands but that’s because there have been so many barriers regarding interoperability, access to broadband and the state of IT in our hospitals.”
Dr Bartone said the AMA had been forced to defend the overarching merits of the MHR service due to the government’s own “poor” communications strategy.
“The reason you might think that I’m actually the front-man for the government on their promotion and campaign is because it’s been done so poorly. This is a clinical tool which we believe has clinical merit. Let’s start from there,” he said.
“We don’t want the last 10 years to be all in vain – that’s why we’re having this conversation. The communications strategy by the authority leaves a lot to be desired, so we’re filling that void because we still see that there is utility in the product.
“It’s the start of an even longer trek – it’s not going to be solved overnight.”
Do you know more? Contact James Riley via Email.

